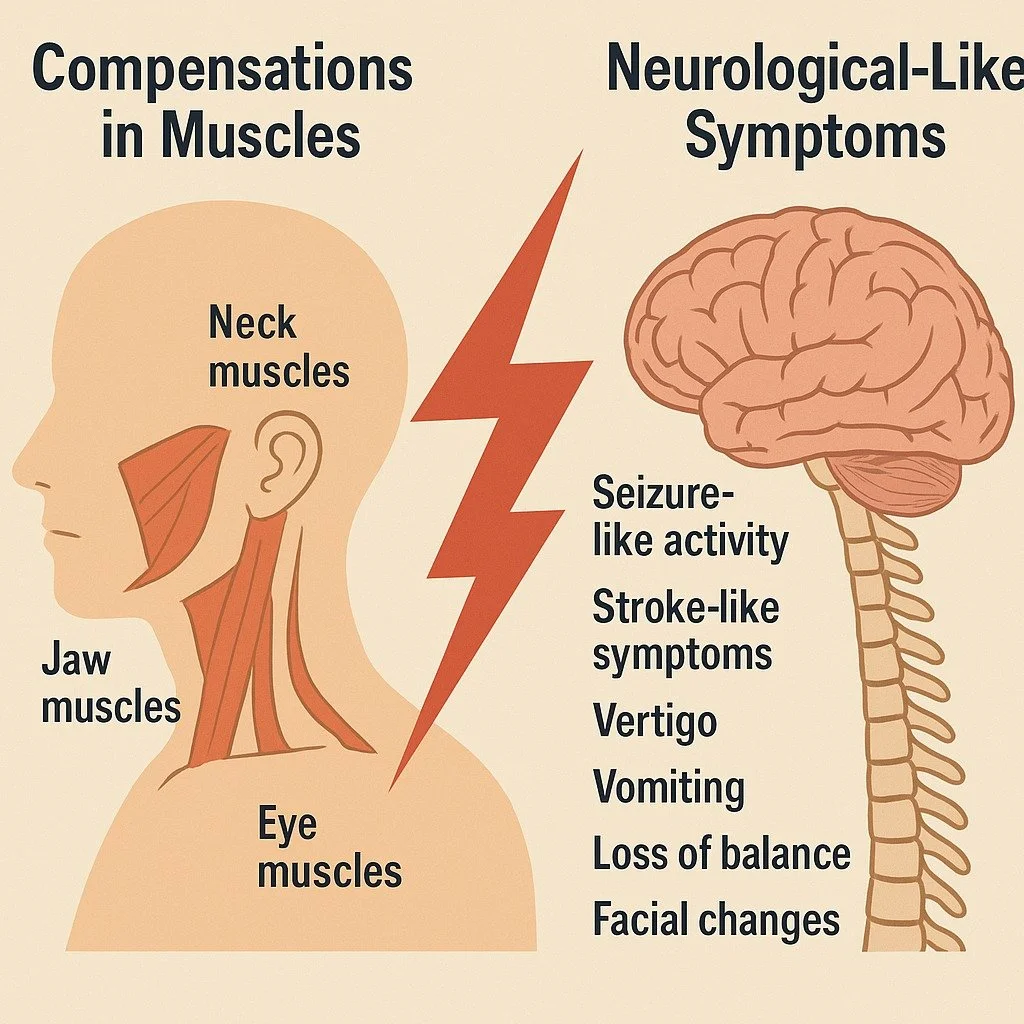
When Neck, Jaw, and Eye Muscle Compensation Creates Neurological-Like Symptoms
Many individuals experience episodes of dizziness, imbalance, facial tension, visual disturbances, nausea, vertigo, or sudden waves of autonomic stress—yet their imaging, labs, and neurological evaluations often return “normal.” These symptoms can be frightening and are sometimes mistaken for stroke, TIA, seizure activity, or other serious neurological events.
While true emergencies must always be ruled out, an overlooked contributor to these symptoms involves neuromuscular compensation—how the neck, jaw, and eye muscles coordinate with one another and how they communicate with the nervous system.
How Neuromuscular Compensation Creates Distressing Symptoms
The neck, jaw, and eye muscles form a tightly interconnected system that helps regulate posture, balance, visual orientation, and head positioning. When certain muscles are under-functioning—due to injury, dental changes, poor posture, scar tissue, or nutritional factors—other muscles often compensate with excessive force.
This can create:
Abnormal tension around sensitive nerves
Irritation of proprioceptive and balance receptors
Altered head/eye tracking
Autonomic system overreactions
Sudden episodes of dizziness, nausea, or disorientation
These patterns can feel neurological, even when no structural neurological problem is present.
Common symptoms linked to these neuromuscular patterns include:
Vertigo or spinning sensations
Loss of balance
Visual strain or difficulty focusing
Facial asymmetry or tension
Nausea or vomiting
“Electrical,” buzzing, or pressure sensations in the head or face
Episodic weakness or collapse sensations
Because imaging is typically static, it does not show what happens when the person is walking, turning their head, reading, or driving—activities in which the symptoms often occur.
Why These Symptoms Are Frequently Misunderstood
Neck, jaw, and eye muscle dysfunction can produce symptoms that resemble neurological disorders, yet they fall outside the scope of most standard medical tests.
A musculoskeletal compensation pattern may:
Overwhelm the body’s balance centers
Disrupt normal neural signaling
Create sudden autonomic shifts
Trigger “false alarms” sensed as neurological events
This is why many individuals are told their symptoms are unrelated, “non-specific,” anxiety-based, or unexplained—even when the underlying neuromuscular issue is correctable.
The Role of Neuromuscular Restoration
A Neuromuscular Restoration Specialist evaluates the muscular system much like an electrician checks a breaker box—identifying which muscles are receiving clear input from the brain, which are overloaded, and which are not communicating well at all.
Through precise manual muscle testing, they can determine:
Which muscles are compensating
Which stabilizers are underactive
How the eyes, jaw, and cervical muscles are coordinating
What primary drivers (injury, dental work, scar tissue, lifestyle habits, nutritional deficits) are creating the imbalance
Once identified, simple corrective exercises and neuromuscular re-patterning techniques can help restore proper muscle function and more accurate neural communication.
Many clients experience significant improvement—often after months or years of inconclusive diagnostics—because the true cause of their symptoms lies in dysfunctional neuromuscular patterns rather than structural disease.
What Typically Drives These Imbalances
Common contributors include:
Whiplash or past neck injuries
Dental procedures or bite changes
Scar tissue from previous surgeries
Excessive screen time or reading
Postural strain from driving or desk work
Nutritional deficiencies affecting nerve and muscle function
Long-standing compensation patterns elsewhere in the body
This is a pattern frequently observed—and often reversible—once the underlying neuromuscular imbalance is correctly identified and addressed.