An Overlooked Component of Pelvic Floor Dysfunction
Chronic pelvic floor discomfort affects many people, yet the underlying cause is often misunderstood. Individuals may experience pain in the pelvic floor muscles, groin, testicles, vagina, or rectal region, along with symptoms such as urinary urgency or incontinence, recurrent UTIs, or discomfort during intercourse. For some, symptoms persist for years without clear answers. Others undergo invasive procedures or traditional pelvic floor therapy, sometimes with only limited relief.
While structural or medical causes must always be ruled out, a lesser-known contributor involves neuromuscular compensation—how the brain communicates with and coordinates the body’s muscular system.
How Neuromuscular Compensation Can Create Pelvic Floor Symptoms
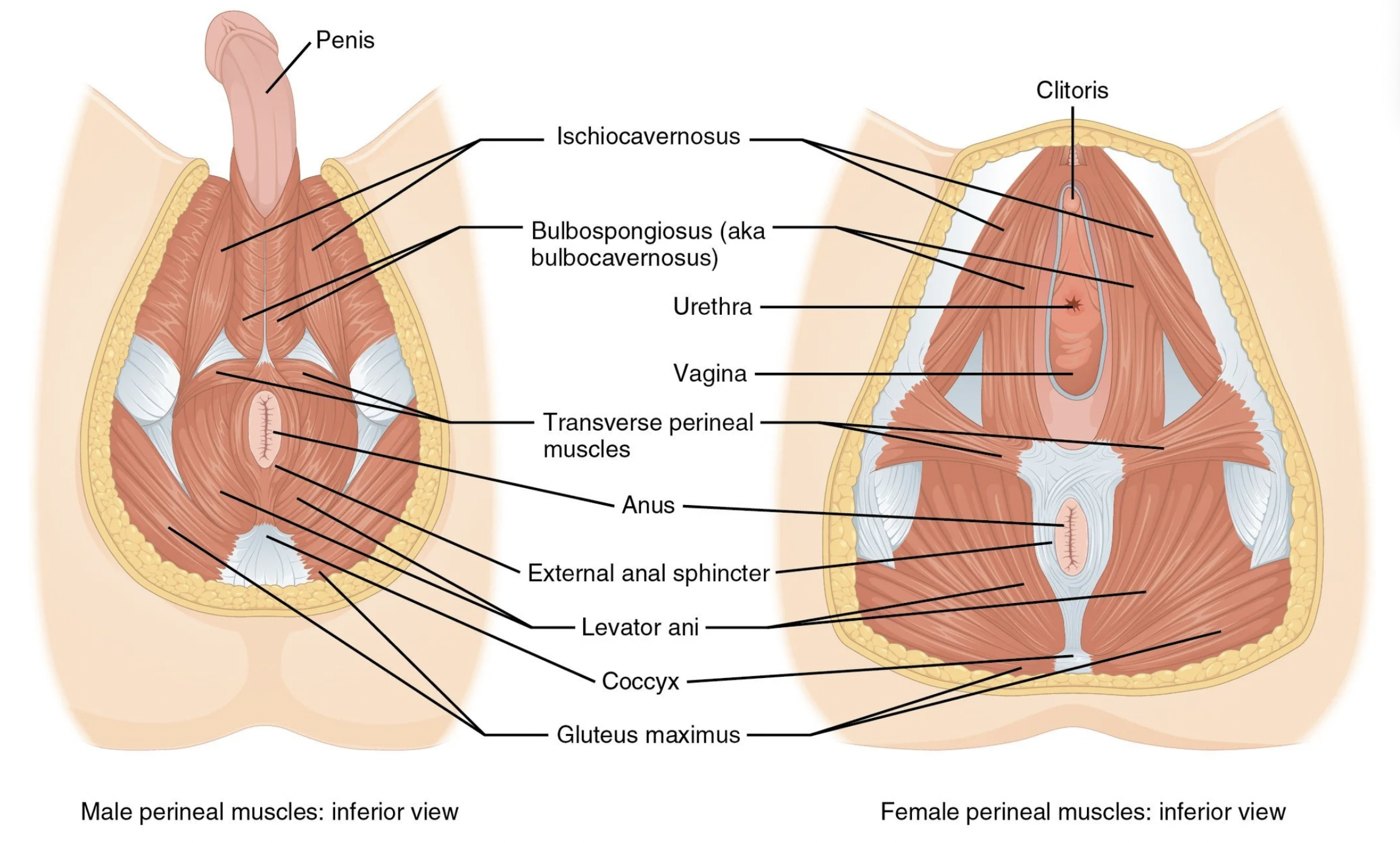
The pelvic floor rarely works in isolation. It collaborates with the abdominal muscles, lumbar stabilizers, diaphragm, and glutes to support posture, movement, continence, and pelvic organ function. When one of these key muscle groups is under-activated, overloaded, or poorly coordinated, the pelvic floor may step in to compensate.
Over time, this can lead to:
Excess tension or pressure in the pelvic floor
Pain in the groin, low abdomen, tailbone, or genital region
Dysfunction during daily movement
Increased strain during activities such as sitting, lifting, or intercourse
Heightened sensitivity due to local muscular overwork
Because these neuromuscular patterns aren’t visible on imaging, they are often overlooked in standard evaluations.
Why This Is Frequently Missed
Most assessments focus on the pelvic region itself, rather than the full neuromuscular network that supports it. However, when the connection between the brain, nerves, and muscles becomes inefficient—whether from injury, lifestyle factors, or prolonged stress—the body redistributes effort. As a result, the pelvic floor may tighten or brace as a protective response.
A neuromuscular restoration specialist evaluates these patterns the way an electrician evaluates circuits—identifying which muscles are receiving clear, efficient input from the brain and which are not. When primary stabilizers such as the abdominal wall, deep lumbar muscles, or glutes are under-functioning, the pelvic floor often bears the extra load.
Common Triggers of Dysfunctional Patterns
Neuromuscular pelvic floor compensation may stem from:
Rapid or extreme dietary changes
Increased alcohol or caffeine intake
Pelvic injuries or childbirth
Long periods of sitting or driving
Scar tissue from surgeries
Excessive Kegel routines
Exercise habits that create imbalance
Lifestyle patterns that overload certain muscle groups
Each of these can disrupt how the body organizes movement and stability.
A Different Approach: Neuromuscular Restoration
At Healing with Excellence, the Neuromuscular Restoration modality addresses pelvic floor dysfunction by examining the entire system—not just the pelvic muscles themselves.
This approach is:
Non-invasive: You remain fully clothed.
Comfortable: No internal examinations, poking, or probing.
Targeted: Simple manual muscle assessments identify which muscles are not communicating effectively with the brain.
Holistic: We evaluate the broader contributors—diet, posture, lifestyle, and compensation patterns—to pinpoint the true drivers of dysfunction.
By restoring efficient neuromuscular communication and reducing unnecessary tension on the pelvic floor, many individuals experience meaningful relief and improved function—often with less discomfort and effort than traditional methods require.
*The information shared here discusses common factors related to your concern and is meant for educational purposes only. It is not a medical diagnosis or a replacement for professional medical care. Everyone’s body is different, and personalized support or a neuromuscular evaluation may be needed for the best results. Your Neuromuscular Restoration Specialist can support and advocate for you while working alongside your medical providers.